TEC and Vitamin D
TAMING TOXIC ERYTHEMA OF CHEMOTHERAPY WITH HIGH-DOSE VITAMIN D

By Warren R. Heymann, MD, FAAD
Feb. 28, 2024
Vol. 6, No. 9
In 2008, Bolognia et al published their landmark editorial introducing the umbrella term TEC. Previously, clinical diagnoses (acral erythema, hand-foot syndrome, erythodysesthesia, intertriginous eruption of chemotherapy, and others) or histologically-based entities (eccrine squamous syringometaplasia, chemotherapy-associated neutrophilic eccrine hidradenitis, and others) were reported and, understandably, might have been construed as distinct disorders. The recognition that TEC is a nonimmunologic toxic phenomenon provided a framework for diagnosing and managing this adverse reaction to chemotherapy. (1)
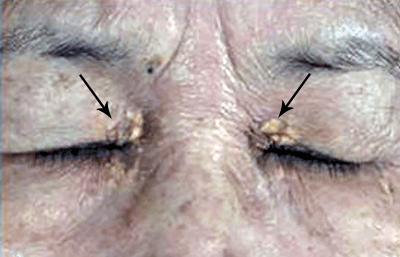
Chemotherapeutic agents such as cytarabine, doxorubicin, docetaxel, capecitabine, and 5-fluorouracil are among the most frequently reported agents causing TEC. (2) In the appropriate context and characteristic clinical presentation, TEC may be diagnosed clinically. TEC may be differentiated from severe forms of intertrigo, SDRIFE (systemic drug-related intertriginous and flexural exanthem), and pemphigus (3) based on history, biopsy, direct immunofluorescence, and serological tests. Tamazian et al reported the case of a 15-month-old boy with acute myeloid leukemia presenting with new onset bilateral erythema of his conchal bowls (in addition to a truncal eruption) a week after administration of cytarabine monotherapy; this resolved with discontinuation of cytarabine and treatment with triamcinolone but recurred with re-administration of cytarabine. Previous reports of TEC affecting the ears have been named "Ara-C ears." (4) Rarely, TEC may mimic toxic epidermal necrolysis (TEN) in which case a biopsy is indicated, demonstrating epidermal dysmaturation and vacuolar alteration in the former and full thickness necrosis in the latter. (5,6) Differentiating TEC from TEN is critical for management decisions.
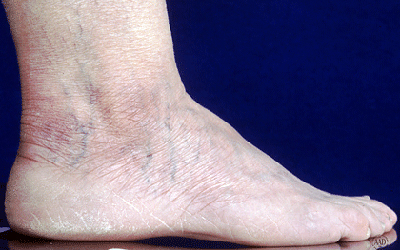
The pathogenesis of TEC is presumably due to eccrine gland secretion of chemotherapeutic agents with resultant localized cytotoxic effects. The most commonly affected sites of TEC correlate with the high concentrations of eccrine glands, such as the palms and soles, and sites of occlusion, notably intertriginous areas. TEC occurs in a dose-dependent manner and may develop several weeks after initiating chemotherapy. TEC resolves spontaneously within 1-4 weeks, and treatment is primarily directed toward managing symptoms. (4)

Symptomatic treatment includes wound care, alcohol-free emollients, elevation, cool compresses, topical steroids, and pain medication. Often chemotherapy dose intensity modification or reduction is necessary if the chemotherapeutic agent cannot be discontinued or substituted for another cancer drug or therapy. (2,4)
According to Ernst et al, "Cholecalciferol (vitamin D3[VitD3]) has recently emerged as a critical immunomodulatory hormone with regulatory roles in the innate and adaptive immune systems. The biologically active form of VitD, calcitriol (1,25[OH]2D3), binds to the ubiquitously expressed VitD receptor and has mechanisms of inflammatory control including expansion of antiinflammatory M2 macrophages, inhibition of proinflammatory NF-κB signaling, and upregulation of arginase-1, an antiinflammatory factor involved in tissue repair." (7) AlGhamdi et al demonstrated that a single bolus of 80,000 IU reduces levels of IL-6, IL-8, and tumor necrosis factor within a month in both men and women. (8,9) In a randomized controlled trial, Annweiler et al observed that early administration of high-dose (400,00 IU) versus standard-dose (50,000 IU) vitamin D3 to at-risk older patients with COVID-19 improved overall mortality at 14 days, however the effect was no longer observed after 28 days. (10)
In their intriguing study, Ernst et al performed a randomized, double-blinded, placebo-controlled interventional trial of healthy human adults, by investigating the clinical and molecular immunomodulatory effects of a single high dose of oral vitamin D3 on an experimentally induced chemical rash. Cutaneous inflammation was induced with topical nitrogen mustard (NM) in 28 participants. Over the next week, participant-specific inflammatory responses to NM alone were characterized using clinical measures, serum studies, and skin tissue analysis. All participants underwent repeat NM exposure to the opposite arm and then received a placebo or 200,000 IU cholecalciferol intervention. The complete rash reaction was followed by multi-omic analysis, clinical measures, and serum studies over 6 weeks. Cholecalciferol mitigated acute inflammation in all participants and achieved 6 weeks of durable responses. Integrative analysis of skin and blood identified an unexpected divergence in response severity to NM, corroborated by systemic neutrophilia and significant histopathologic and clinical differences. Multi-omic and pathway analyses revealed a 3-biomarker signature (CCL20, CCL2, CXCL8) unique to exaggerated responders suppressed by cholecalciferol, thereby implicating IL-17 signaling involvement. The authors concluded that high-dose systemic cholecalciferol may be an effective treatment for severe reactions to topical chemotherapy. Their findings have broad implications for vitamin D3 as an anti-inflammatory therapy that hinders development of exaggerated immune responses. (7) Future therapeutic studies of high-dose vitamin D for severe drug eruptions such as TEN, acute generalized exanthematous pustulosis, and others can be anticipated.
Nguyen et al treated 6 patients with TEC with high dose vitamin D (50,000 IU in 1 patient, 100,000 IU in 5 patients) with a mean [range] time to first administration from rash onset of 4.3 [1-7] days. The dose was repeated in 7 days. Topical corticosteroids were also prescribed. All patients experienced symptomatic improvement in pain, pruritus, or swelling by the next day and improvement in redness within 1 to 4 days. (11) If these findings can be confirmed, using vitamin D to shorten the course of TEC would offer relief and presumably allow continuation of chemotherapy.
In conclusion, dermatologists should recognize the classical features of TEC and consider the diagnosis in atypical cases for patients on chemotherapy. Although most therapeutic measures focus on supportive care, new data suggests that high-dose vitamin D may be therapeutic.
Point to Remember: Toxic erythema of chemotherapy (TEC) is the umbrella term for multiple eruptions caused by chemotherapeutic agents. TEC may last for up to a month. Although confirmatory studies are warranted, research suggests that the anti-inflammatory action of high-dose vitamin D may be of therapeutic value in TEC.
Our expert's viewpoint
Jean L. Bolognia, MD, FAAD
Vice Chair of Faculty Affairs, Professor of Dermatology
Yale School of Medicine
The 2008 editorial to which Warren alludes came together because of contributions from my husband, Dennis Cooper, a hematologist-oncologist who specializes in hematopoietic stem cell transplantation, and an insightful dermatopathologist, Earl Glusac. In patients with multiple sites of involvement, including the major body folds, knees, and even the ears, the problem with using the term "hand-foot syndrome" is as follows: At the time of initial consultation, there may be burning and erythema of the palms and soles, but a few days later one is asked to address dusky erythema of the axillae and groin with prominent moist desquamation. Now the dermatologist can't say "hand-foot syndrome" of the major body folds (which is even more troublesome than diagnosing a primary cutaneous diffuse large B-cell lymphoma, leg type but not on the legs). Misdiagnoses such as cutaneous candidiasis are then made even though the patient is on week three of posaconazole. Of note, in patients with darker skin phototypes, it is the erosive desquamation that often points to the diagnosis of TEC.
Because there can be overlap histologically with GVHD plus chemotherapeutic changes, generalized bullous fixed drug eruption, or SJS/TEN, it is the clinician who makes the final diagnosis. The clinical recognition of TEC is based upon the distribution pattern, what I refer to as the "low-power" examination of the skin. The symmetry (unless a site has been irradiated), the buck shot that surrounds a larger central lesion (e.g., on the central knees), the preference for major body folds, and in men, a nearly universal burning scrotum with agents such as busulfan, lead to the diagnosis. Because the interval between administration of the conditioning regimen and TEC is often weeks, the link between the chemotherapy and the eruption may be unrecognized; it is likely that a number of the patients previously diagnosed with palmoplantar GVHD actually had TEC. Occasionally, more severe TEN-like disease can be seen when full doses of renally excreted drugs are given in the setting of impaired kidney function or multiple high-risk drugs are combined. Again, the initial distribution pattern is the clue to diagnosing TEC.
Bolognia JL, Cooper DL, Glusac EJ. Toxic erythema of chemotherapy: a useful clinical term. J Am Acad Dermatol. 2008 Sep;59(3):524-9. doi: 10.1016/j.jaad.2008.05.018. PMID: 18694683.
Chidharla A, Kanderi T, Kasi A. Chemotherapy Acral Erythema. 2022 Mar 6. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022 Jan–. PMID: 29083584.
Pathania YS, Budania A. Toxic erythema of chemotherapy. QJM. 2021 Nov 5;114(8):611-612. doi: 10.1093/qjmed/hcab136. PMID: 33989410.
Tamazian S, Oboite M, Larijani M, Oliver B, Milbar H, Jen M, Treat JR. Toxic erythema of chemotherapy affecting the ears of an infant: A case report. Pediatr Dermatol. 2021 Mar;38(2):512-513. doi: 10.1111/pde.14522. Epub 2021 Jan 22. PMID: 33481261.
Birmingham SW, Moon DJ, Kraus CN, Lee BA. Enfortumab Vedotin-Associated Toxic Epidermal Necrolysis-like Toxic Erythema of Chemotherapy. Am J Dermatopathol. 2022 Dec 1;44(12):933-935. doi: 10.1097/DAD.0000000000002255. Epub 2022 Jul 19. PMID: 35925560.
Mehta H, Mete UK, Gupta P, Ranjan KR, Nahar Saikia U, Mahajan R. Toxic epidermal necrolysis-like presentation of toxic erythema of chemotherapy. Clin Exp Dermatol. 2022 Jun;47(6):1201-1203. doi: 10.1111/ced.15165. Epub 2022 Apr 1. PMID: 35262213.
Ernst MK, Evans ST, Techner JM, Rothbaum RM, Christensen LF, Onay UV, Biyashev D, Demczuk MM, Nguyen CV, Honda KS, McCormick TS, Tsoi LC, Gudjonsson JE, Cooper KD, Lu KQ. Vitamin D3 and deconvoluting a rash. JCI Insight. 2023 Jan 24;8(2):e163789. doi: 10.1172/jci.insight.163789. PMID: 36692020.
AlGhamdi SA, Enaibsi NN, Alsufiani HM, Alshaibi HF, Khoja SO, Carlberg C. A Single Oral Vitamin D3 Bolus Reduces Inflammatory Markers in Healthy Saudi Males. Int J Mol Sci. 2022 Oct 9;23(19):11992. doi: 10.3390/ijms231911992. PMID: 36233290; PMCID: PMC9569869.
Alsufiani HM, AlGhamdi SA, AlShaibi HF, Khoja SO, Saif SF, Carlberg C. A Single Vitamin D3Bolus Supplementation Improves Vitamin D Status and Reduces Proinflammatory Cytokines in Healthy Females. Nutrients. 2022 Sep 24;14(19):3963. doi: 10.3390/nu14193963. PMID: 36235615; PMCID: PMC9570631.
Annweiler C, Beaudenon M, Gautier J, Gonsard J, Boucher S, Chapelet G, Darsonval A, Fougère B, Guérin O, Houvet M, Ménager P, Roubaud-Baudron C, Tchalla A, Souberbielle JC, Riou J, Parot-Schinkel E, Célarier T; COVIT-TRIAL study group. High-dose versus standard-dose vitamin D supplementation in older adults with COVID-19 (COVIT-TRIAL): A multicenter, open-label, randomized controlled superiority trial. PLoS Med. 2022 May 31;19(5):e1003999. doi: 10.1371/journal.pmed.1003999. PMID: 35639792; PMCID: PMC9154122.
Ernst MK, Evans ST, Techner JM, Rothbaum RM, Christensen LF, Onay UV, Biyashev D, Demczuk MM, Nguyen CV, Honda KS, McCormick TS, Tsoi LC, Gudjonsson JE, Cooper KD, Lu KQ. Vitamin D3 and deconvoluting a rash. JCI Insight. 2023 Jan 24;8(2):e163789. doi: 10.1172/jci.insight.163789. PMID: 36692020.
Nguyen CV, Zheng L, Zhou XA, Ernst MK, Kye Y, Choi JN, Lu KQ. High-Dose Vitamin D for the Management of Toxic Erythema of Chemotherapy in Hospitalized Patients. JAMA Dermatol. 2023 Feb 1;159(2):219-222. doi: 10.1001/jamadermatol.2022.5397. PMID: 36542397; PMCID: PMC9856756.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
DW Insights and Inquiries archive
Explore hundreds of Dermatology World Insights and Inquiries articles by clinical area, specific condition, or medical journal source.
Skin Care Physicians of Costa Rica
Clinica Victoria en San Pedro: 4000-1054
Momentum Escazu: 2101-9574
Please excuse the shortness of this message, as it has been sent from
a mobile device.
posted by dermatica at
February 28, 2024
|
0 Comments
![]()
![]()