Usos no tradicionales de farmacos tradicionales
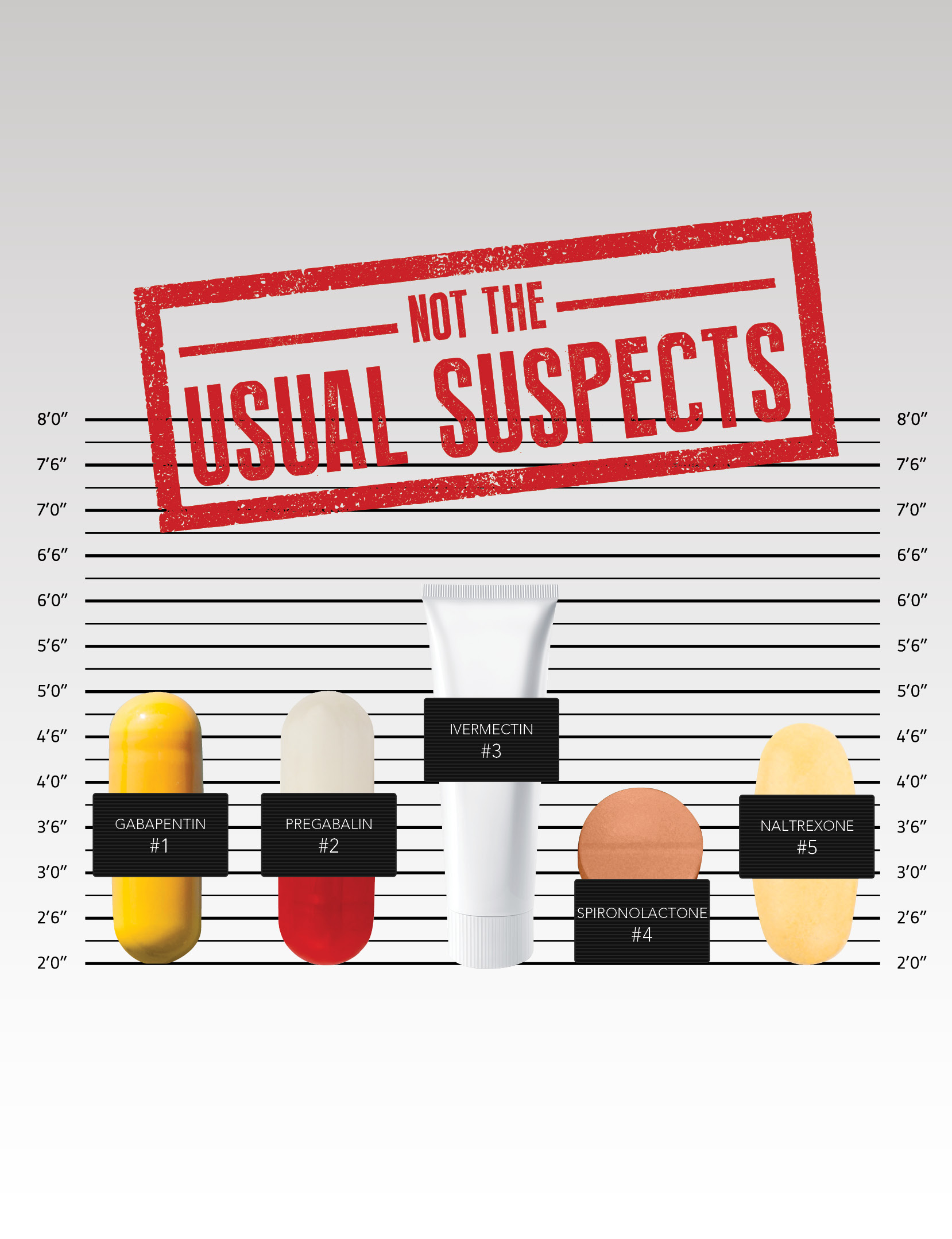
NOT THE USUAL SUSPECTS
Drugs you never thought you'd use in dermatology
By Jan Bowers, contributing writer
Young dermatologists quickly become familiar with mainstays of treatment such as antibiotics, corticosteroids, and antihistamines. However, when those therapies fail, or when conditions dictate a novel approach, less common agents can play a key role in the treatment of acne, rosacea, pruritus, and other skin disorders. Dermatology World spoke with four dermatologists about their experiences and research in treating selected patients with:
- Gabapentin and pregabalin
- Ivermectin
- Spironolactone
- Naltrexone
ATTACKING CHRONIC ITCH
Two anticonvulsant medications that have been used to manage chronic pain are also proving effective in the treatment of selected types of chronic itch: gabapentin and pregabalin.
"Chronic pain and chronic itch have a lot of similarities," said Gil Yosipovitch, MD, professor of dermatology at the University of Miami Miller School of Medicine and director of the Miami Itch Center. "This is one of the mainstay treatments that I use for patients who have chronic itch of different types."
Dr. Yosipovitch cited neuropathic itch, a result of nerve damage, and itch caused by neural sensitization as two types that respond well to gabapentin and pregabalin. "People with atopic dermatitis, for example, have a neural sensitization phenomenon, meaning the nerves are hyperactive — they're very sensitive, and they fire more than a normal nerve," he explained. "What the gabaergic drugs do is reduce that hyperactivity. They were designed initially for epilepsy, where there's a lot of electric activity of the nerves. They're now prescribed for many different kinds of pain, so it makes sense to use them in chronic itch associated with neural sensitization, as well as for neuropathic itch."
Efficacy
In a clinical review of the mechanism of and therapeutic approaches to itch (J Allergy Clin Immunol. 2018;142(5):1375-139), Dr. Yosipovitch listed prurigo nodularis, postburn pruritus, uremic pruritus, and paraneoplastic pruritus, in addition to neuropathic itch, as indications for the use of anticonvulsant systemic therapies. Other conditions shown to respond to these drugs, according to a review of published studies (J Am Acad Dermatol. 2016;75:619-25), include brachioradial pruritus, notalgia paresthetica, and scalp dysesthesia, among others. The JAAD authors noted that among the conditions studied, uremic pruritus appeared to be the most responsive to these agents.
The gabaergic drugs work on interneurons, an inhibitory system in the spinal cord that may also be in the brain, Dr. Yosipovitch explained. "They most probably inhibit the overactivity of the nerve. They don't inhibit the nerves from acting; they don't block all transmission. However, the intensity of the transmission goes down significantly. They don't inhibit itch specifically; rather, they work on spinal nerve fibers, which can transmit both itch and pain."
Dosing
Dosing depends on the age of the patient and the underlying conditions — and pregabalin is given less frequently and at lower doses than gabapentin, Dr. Yosipovitch said. For gabapentin, "I start with a low dose of 300 milligrams and increase it gradually every two days by another [300 mg] tablet. I usually start it at nighttime, because this drug initially causes significant sleepiness." In patients with kidney failure who are on dialysis, "you give low doses, like three times a week, after dialysis. In younger folks that I see sometimes who have significant neuropathic damage, I start with 600 milligrams."
Gabapentin is usually given three or four times a day, but "with pregabalin it's only twice a day, and the doses are much lower. The maximum dose I usually give is 300 milligrams a day — it could be 400 — and the minimum could be 25 to 50 milligrams." Pregabalin is easier to use because it requires fewer doses, Dr. Yosipovitch pointed out, but "it's more expensive, so insurance companies would prefer that we don't allow a lot of patients to be on pregabalin without first using gabapentin." Another factor in choosing between the two agents is that some patients who fail gabapentin will respond to pregabalin, and vice versa. "I don't have any explanation in terms of pharmacology. The drugs work on the same receptors," Dr. Yosipovitch said. "There are no studies that compare the two head to head. It just shows that our human bodies are unique."
Side effects
In addition to drowsiness, adverse events include dizziness and swelling of the legs, Dr. Yosipovitch noted. "The swelling is not putting patients at risk in any way, but it's important to understand. In some patients, there is constipation and GI complaints, but overall, these two drugs are now used by millions of patients." As one of the first dermatologists to use gabaergic drugs to manage itch, Dr. Yosipovitch said that unlike the situation 10 years ago when, "I could count the number of dermatologists using them on two hands, now, I would say that most dermatologists are at least aware of them." Some are hesitant to give patients doses above 300 milligrams, "but experts usually give higher doses that go up to 3 grams and more. Patients come to me and say, 'they gave me gabapentin, one pill,' so 100 or 300 milligrams. That's not a dose that would usually work for these types of itch, so that's one of the challenges."
DEADLY TO DEMODEX
Many dog owners are familiar with ivermectin as the active ingredient in their pet's heartworm medicine. In humans, it can be administered orally to treat parasitic diseases such as onchocerciasis (river blindness) and strongyloidiasis, and topically, in a 0.5% formulation, to eliminate head lice. This versatile antihelmintic is also proving to be effective in treating the lesions of moderate-to-severe papulopustular rosacea (PPR) by targeting Demodex folliculorum, a mite that populates the human face.
"We're all colonized with Demodex within 24 hours of birth," said Zoe Diana Draelos, MD, a private practitioner in High Point, North Carolina, and a consulting professor of dermatology at Duke University. "People with rosacea are unique in that they may have more mites on their face — not always — but they seem to have more of an immune response to the mites. The question is whether the mites cause the inflammation or whether the inflammation reduces the immune system and allows the proliferation of the mites. We know the mites are very important because ivermectin acts as an anti-inflammatory but also as an anti-mite agent."
An elongated parasite, Demodex "sit with their heads down in the sebum-containing pore utilizing human sebum as a nutritional source. The mites release their waste products, which are composed of free fatty acids, into the pore and surrounding tissues, which are extremely irritating," Dr. Draelos explained. "Free fatty acids are released not only by Demodex, but also by bacteria like Proprionibacterium acnes, which is the causative agent in acne. It's interesting that all organisms that utilize sebum as a nutritional source release free fatty acids, and providing a common pathway for inflammation, not only in rosacea, but also in inflammatory acne and in the facial erythema and desquamation associated with seborrheic dermatitis." Just as the causes of rosacea are not clearly understood, it's not known why people who do not have PPR don't react in the same way to the release of the free fatty acids, Dr. Draelos noted. "Either we don't have as many of the Demodex organisms, or our immune systems are not as responsive."
Efficacy and dosing
The results of two randomized, double-blind studies (J Drugs Dermatol. 2014;13(3):316-23) showed that a 1% ivermectin cream was superior to vehicle cream in achieving treatment success (Investigator's Global Assessment "clear" or "almost clear") and reducing inflammatory lesion counts. Dr. Draelos, who co-authored publication of the studies, recommends a "pulsing" method of ivermectin treatment. "You may want to treat the patient daily with ivermectin until clearing. Usually you see some clearing between four and eight weeks," she remarked. "Once the Demodex are gone, they will repopulate if you don't do something. Then you could go down to once a week, and if you don't get a recurrence, reduce it to once every two weeks. Many people can be maintained on one treatment a month." Ivermectin can be used in combination with oral antibiotics, which can resolve rosacea more rapidly, Dr. Draelos added. "The tetracycline family of antibiotics is anti-inflammatory, but also kills bacteria in the gut of the Demodex. And some researchers think it's not just the presence of the Demodex but also the bacteria in its gut that causes people to develop the inflammation associated with rosacea."
Side effects
Dr. Draelos characterized ivermectin as "very safe," and the two randomized studies found no serious adverse events related to ivermectin. "When you hear that it's an antiparasitic, you might think that it's a very strong, dangerous medication, but the safety profile post-drug approval has been excellent, and there haven't been any major issues that have arisen."
In her view, the biggest challenge facing its use is that it's not first-line therapy on most formularies, and it can be expensive. "I think ivermectin is probably, in most areas, either second or third tier. That's why tapering off the medicine and finding out the minimum amount of application that will keep patients clear is very important for dermatologists to recognize, because that allows the patient to get as much value as possible from their medication purchase."
SPIRONOLACTONE AS ANTIANDROGEN
Spironolactone is a triple threat against acne, Dr. Reynolds said. "It inhibits the 5-alpha reductase activity in the hair follicle and sebaceous glands. It blocks androgen receptors on the hair follicle and sebaceous glands, and it can slightly reduce testosterone production, so its effectiveness for hirsutism and acne is really by acting as an antiandrogen." She added that the evidence for its efficacy against alopecia is less strong than that for acne and hirsutism, "but it's something that I've certainly tried in my patients with female pattern hair loss, with some success, and there is some support for it in the literature."
Efficacy
In a review of the use of oral spironolactone in post-teenage female patients with acne (J Clin Aesthet Dermatol. 2012;5(3):37-50), the authors note that the drug "has been used frequently in the dermatology clinic for women with hormonal-pattern acne vulgaris, defined clinically as primarily inflammatory papules, many deep-seated and tender, that are located predominantly on the lower half of the face and anterior-lateral neck region." Dr. Reynolds said that spironolactone and oral contraceptive pills can be helpful in all females with acne, "even if they don't have an androgen excess disorder. The vast majority of studies that have been done looking at the efficacy of these hormonal agents in acne are looking at an across-the-board female population. I would say that where spironolactone fits into the armamentarium [of acne therapies] would be for a woman who has failed topical therapy." The authors of the most recent AAD acne guidelines (J Am Acad Dermatol. 2016;74(5):945-73) noted a lack of data to support the efficacy of spironolactone in the treatment of acne, but concluded that despite this, "relying on available evidence, experience, and expert opinion, the work group supports the use of spironolactone in the management of acne in select women."
Dosing
The effective dose of spironolactone for acne is generally lower than that required to treat hirsutism or hair loss, Dr. Reynolds said. "For acne, you can see efficacy in a dose as low as 25 milligrams a day, but you may have to go up to as high as 100 milligrams twice a day. For acne, it usually works quickly, in two to three months. For hirsutism, you tend to need higher doses, like up to that 100-milligram, twice a day dose, and it may take at least six months to see the benefit. For female pattern hair loss, again, the studies that were done used doses of 100 milligrams twice a day. They saw some benefit at six months, but generally you would want to give it at least a year to determine if it's efficacious." According to her research, women who have polycystic ovarian disease may require higher doses of spironolactone to control their acne than those who do not have the disorder, Dr. Reynolds noted. Spironolactone can be given as monotherapy or in combination with oral contraceptives and/or antibiotics.
Side effects
Spironolactone is generally well-tolerated, but it can cause menstrual irregularities (the most common side effect), breast tenderness, and gastrointestinal effects, Dr. Reynolds said. "These side effects are dose-related," she noted. "Since it is a diuretic, women will experience increased urination and could experience lightheadedness and headaches, so it's important to keep up with fluid intake." It should not be used in patients who have kidney failure, those who are taking other medications that cause hyperkalemia, or those who are pregnant or breastfeeding.
Aside from those contraindications, dermatologists should give it a try, Dr. Reynolds suggested. "I think they'll be impressed at how efficacious it can be in their patients who have had stubborn acne that's been refractory to other therapies, especially those who have relapsed after a course of isotretinoin, which does not address the hormonal component of acne."
A PARADOXICAL EFFECT
An opioid antagonist first synthesized in 1963, naltrexone has traditionally been used to treat opioid and alcohol addiction, for which it is usually given orally in 50- to 100-milligram doses. However, a much lower dose of 1-5 milligrams is showing efficacy against a range of skin disorders that are notoriously refractory to treatment.
Efficacy
Dosing
Side effects
Overall, Dr. Elston maintained, "as long as your patient is not being treated with narcotics, where you would interfere with that therapy, it is reasonable to try naltrexone in many of these conditions where other options simply aren't working."
Skin Care Physicians of Costa Rica
Clinica Victoria en San Pedro: 4000-1054
Momentum Escazu: 2101-9574
Please excuse the shortness of this message, as it has been sent from
a mobile device.
posted by dermatica at
November 14, 2019
![]()
![]()

0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home