10 Years of Studies Link Acne Breakouts to Diet
Key Takeaways
- A new review of studies aims to prove diet can play a role in acne development.
- While the data is still evolving, avoiding chocolate, soda, and dairy might be protective against acne.
A review of 10 years of studies and clinical trials shows that what you eat might play a role in whether or not you develop acne.1 The review, which was published in the International Journal of Dermatology in February 2021, aims to put an end to the question of whether acne and diet are related.
"Data like this certainly helps further support the evidence that diet somehow plays a role in treatment of acne patients," Claire O'Bryan, APRN, a nurse practitioner and co-founder of The Skin Clique, tells Verywell.
Since acne can be a source of stress and anxiety for people who have it, O'Bryan, who was not involved with the study, says that being able to combine evidence-based dietary advice with traditional topical treatments will help clinicians treat acne patients holistically.
A Decade Worth of Studies
The researchers performed a systematic review of 11 interventional clinical trials and 42 observational studies that were published over 10 years.1
The results showed that there were several dietary factors associated with acne:
- High glycemic index diet
- High glycemic load diet
- Certain dairy foods
- Fast food
- Chocolate
- Low intake of raw vegetables
However, there were also several dietary patterns that appeared to have a more protective role against acne, including:
- Frequent consumption of fruits and vegetables (more than 3 days per week)
- Fish included in the diet
Although the data was not as strong, the researchers did find evidence suggesting that eating eggs more than three days per week, drinking large amounts of soft drinks, and eating salty food could also be acne-promoting dietary factors.
Can Diet Help Manage Acne?
The role of diet in acne development and presentation is still not completely clear. While many studies suggest that dairy foods are linked to increased acne prevalence, a 2019 study published in the journal Clinical Nutrition found that consumption of certain dairy foods—specifically yogurts and cheeses—had no effect on acne occurrence.2
Among the recommendations in the medical literature regarding diet and acne, the strongest evidence supports limiting refined sugars and high glycemic foods as much as possible.3
What Is a High Glycemic Diet?
A high glycemic diet is a way of eating that is based on how certain foods affect blood sugar levels. High glycemic foods increase blood sugars quickly and trigger excess insulin.
Foods that are considered to be "high glycemic" foods include white bread, sugary desserts, and certain fruits, like watermelon.
Refined carbohydrates, sodas, and ultra-processed foods such as cookies and cake can increase blood sugar levels quickly and trigger a hormonal response—both of which might be related to getting acne.
In fact, data published in 2012 suggested that when people with acne ate a low-glycemic load diet for 10 weeks, they had significantly less acne when compared to people who ate their normal diet.4
Possible Dietary Recommendations For Acne
- Limit refined sugars (table sugar, agave syrup, cane sugar, corn syrup)
- Choose low glycemic foods (whole grains, vegetables, berries, nuts, seeds, and fruits with skin such as pears and apples)
- Avoid chocolate
- Opt for yogurt and cheese if you eat dairy
- Include fish in your diet
- Avoid sugary soft drinks
What Else Causes Acne?
Acne is the eighth most common skin disease in the world. Acne often has a negative effect on the social lives, self-esteem, and body images of people who have it.5
"The thing that makes acne so hard to tackle is that our skin is one of the only organs that reacts both to external and internal stimuli," Meg Hagar, MS, RD, CDN, CLT, CHHP, Licensed Aesthetician and Acne Nutritionist, tells Verywell. "As far as why acne happens, we have to look both at the potential external stimuli and internal stimuli."
While dietary factors appear to play a role in acne appearance, they are not the only factors. Family history, age, skin type, hormones, and cannabis smoking habits may also play a role, according to a systematic review published in Scientific Reports in 2020.5
A few studies in the review found that lack of sleep or insomnia, sun exposure, high mental stress, and using cosmetics might also be associated with increased acne.
No Silver Bullet Acne Treatment
There is no single treatment to target acne that works for everyone. While your diet might be one factor, there are still grey areas in dietary recommendations for people who experience acne.
Research suggests that probiotics could be promising for combatting acne. More specifically, consuming fermented foods (a natural source of probiotics) may offer some benefit.6
If changing your diet does not help, there are still other ways to treat acne. A doctor-recommended topical treatment may also be beneficial.
What This Means For You
Acne is a common condition, but the cause can vary from person to person. This makes it difficult to pinpoint the best treatment for an individual. The role of diet in acne presentation is still being researched, but if you have the condition, it might be worth trying to make certain changes to your diet to see if it helps reduce your acne.
Limiting sugar, choosing low-glycemic foods, and cutting back on dairy are just a few examples of dietary recommendations that might be beneficial if you have acne.




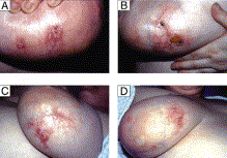 Image from reference 7.
Image from reference 7. 


"Intralesional Antigen Immunotherapy in the Treatment of Periungual Warts" by Nofal and colleagues is a report on a well-designed, well-executed study. They compare intralesional immunotherapy with Candida, MMR, and PPD for the treatment of periungual warts. As dermatologists, we all know how difficult it is to treat warts under and around the nails as well as to eradicate the virus under the nail plate. These authors designed a Skintastic study and report similar efficacy to other studies for the treatment of warts using immunotherapy, which hovers at about 70%. As expected, compared with other studies, Candida immunotherapy is more robust and therefore will have a higher success rate and a higher adverse event rate as compared with MMR. Complete response with Candida is 80% versus 74% with MMR and 70% with PPD. The rate of local adverse events is 12% with Candida, 6% with MMR, and 8% with PPD. Flu-like symptoms occur in 10% of people treated with Candida, 4% with MMR, and 6% with PPD. No patients had recurrence of warts after 6 months. The authors also were able to demonstrate distant response of untreated warts. Their design is like our paper published in 2001, which is one of the first papers to show the benefits of injecting Candida skin test antigen to treat warts.1 This is another well-done paper to support the use of Candidaimmunotherapy for the treatment of HPV tumors.
Reference