IgG4 RD and RSD
The illusions of IgG4-related skin disease

By Warren R. Heymann, MD, FAAD
Dec. 10, 2025
Vol. 7, No. 48

Prior to researching this commentary, I had illusions that I grasped the fundamental concepts of IgG4-related disease (IgG4-RD); after writing this editorial, I have no such illusions — IgG4-RD is a confounding disorder. IgG4-RD is confusing because its manifestations are protean, and its pathogenesis is poorly understood. IgG4-RD is a multi-organ, fibro-inflammatory condition with tumefactive lesions of unknown etiology and characteristic histopathological features. Virtually any organ can be involved; the pancreas, kidneys, orbital adnexal structures, salivary glands, and retroperitoneum are most commonly affected. (1) IgG4-related skin disease (IgG4-RSD) is the focus of this commentary.
Katz and Stone state, "Early diagnosis and treatment of this elusive disease can prevent substantial organ damage from end-stage fibrosis, emphasizing the need for prompt recognition and accurate characterization of IgG4-RD." (2)
The revised comprehensive diagnostic criteria for IgG4-RD consists of 3 domains: 1) Clinical and radiological features, 2) Serological diagnosis, and 3) Pathological diagnosis. The diagnostic criteria (3) are presented below in a table after the references.
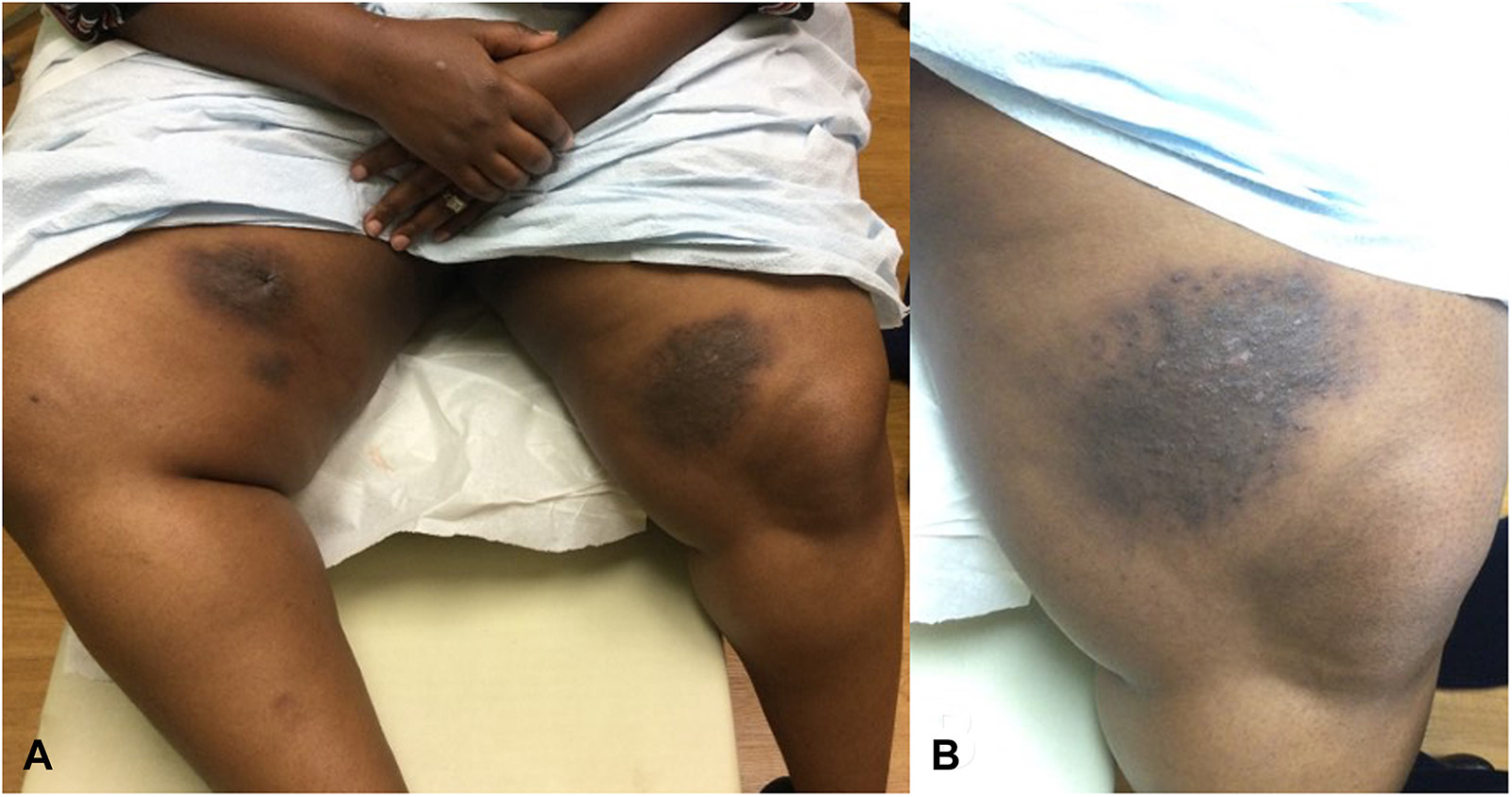
Tokura et al. classify IgG4-RSD in 7 types, the first 3 due to direct infiltration of IgG4(+) plasma cells and types 4 through 7 manifesting as secondary lesions caused by IgG4(+) plasma cells and/or IgG4. The types are: 1) cutaneous plasmacytosis (multiple papulonodules or indurations on the trunk and proximal part of the limbs), 2) pseudolymphoma and angiolymphoid hyperplasia with eosinophilia (plaques and papulonodules mainly on the periauricular, cheek and mandible regions), 3) Mikulicz disease (palpebral swelling, sicca syndrome and exophthalmos), 4) a psoriasis-like eruption (strikingly mimicking psoriasis vulgaris), 5) unspecified maculopapular or erythematous eruptions, 6) hypergammaglobulinemic purpura (bilateral asymmetrical palpable purpuric lesions on the lower extremities) and urticarial vasculitis (prolonged urticarial lesions occasionally with purpura), and 7) ischemic digit (Raynaud phenomenon and digital gangrene). (4)
The following three articles are worthy examples of the clinical variability of IgG4-RSD. Mishlab et al. present a >70-year-old man with nodules and tumors on his trunk and extremities that demonstrated psoriasiform hyperplasia with a lymphoplasmacytic and eosinophilic infiltrate with > 40 IgG4+ plasma cells per high power field. He improved with prednisone and mycophenolate mofetil within a few months. (5) Atasuka et al. report a 69-year-old man with indurated tumors on his cheeks that developed over 6 months. The histologic picture displayed plasma cells and eosinophils with an IgG4/IgG ratio > 40% and elevated serum IgG4. His lesions resolved with prednisone administration. (6) Gitin et al. detailed a 39-year-old HIV+ woman with cutaneous xanthomatous Rosai-Dorfman disease with overlapping features of IgG4-RD. (7)
Clinical-pathologic correlation is essential in securing a diagnosis of IgG4-RSD. Although the histopathologic findings of IgG4-RD are similar in all involved organs (characterized by storiform fibrosis, obliterative phlebitis, and a dense lymphoplasmacytic infiltrate enriched with IgG4+ plasma cells demonstrating an IgG4/IgG ratio of >0.4), the disorder must be differentiated from histologic mimickers (syphilis, marginal zone lymphoma, psoriasis, angiolymphoid hyperplasia with eosinophilia, necrobiosis lipoidica, lichen sclerosus, others). (8)
Therapeutically, IgG4-RD is generally responsive to glucocorticoids. Other immunosuppressive agents have been used. It is not surprising that dupilumab has been reported to be effective as IgG4-RD may be associated with a Th2 profile — this proved to be the case in a 36-year-old man with cholangitis, pancreatitis, interstitial nephritis, and lichen amyloidosis. (9) Small case series and retrospective studies reported the efficacy of rituximab. (10) Stone et al. performed a phase 3, multicenter, double-blind, randomized, placebo-controlled trial, adults with active IgG4-RD who underwent randomization in a 1:1 ratio to receive inebilizumab (a humanized IgG kappa monoclonal antibody that depletes B cells by targeting CD19) or placebo for a 52-week treatment period. Participants in both groups received identical glucocorticoid tapers. Glucocorticoids were allowed to treat disease flares, but background immunosuppressants were not permitted. A total of 135 participants with IgG4-RD underwent randomization: 68 participants were assigned to receive inebilizumab and 67 were assigned to receive placebo. Treatment with inebilizumab reduced flare risk; seven participants (10%) in the inebilizumab group had at least one flare, as compared with 40 participants (60%) in the placebo group (hazard ratio, 0.13; P<0.001). Adverse events were reported in > 10% of those in the inebilizumab group (COVID-19 in 24%, lymphopenia in 16%, and urinary tract infection in 12%). The authors concluded, "Inebilizumab reduced the risk of flares of IgG4-related disease and increased the likelihood of flare-free complete remission at 1 year, confirming the role of CD19-targeted B-cell depletion as a potential treatment for IgG4-related disease." (11) Obexelimab, a biologic agent targeting both CD19 and Fc-gamma-RIIb, has nearly completed enrolment for a phase 3 trial involving approximately 200 patients. (12)
Much has been learned about IgG4-RD and IgG4-RSD since its recognition more than two decades ago. It is gratifying that new approaches may prevent severe complications. B-cell depletion therapy affords exciting new therapeutic opportunities. I will conclude with a more optimistic quote from Stephen Hawkin — "Intelligence is the ability to adapt to change." We are approaching IgG4-RSD intelligently.
Point to Remember: The diagnosis of IgG4-related skin disease requires careful clinical-pathological correlation because of its varied cutaneous presentations. B-cell depletion therapy with biologic agents such as inebilizumab or obexelimab is promising a future surpassing steroid therapy for this disease.
Our expert's viewpoint
Kiran Motaparthi, MD, FAAD
Clinical Professor
Vice Chair of Education
Department of Dermatology
University of Florida College of Medicine
As noted by Dr. Heymann, several dermatologic disorders demonstrate overlapping features with IgG4-RD, including Rosai-Dorfman disease (RDD). Granuloma faciale (GF), erythema elevatum diutinum, and Sjogren syndrome can also be confused with IgG4-RD. While the available sets of criteria include specific numerical thresholds for serum IgG4 levels and IgG4-expressing plasma cells per high power field (hpf), there are caveats to these cutoffs. For instance, some bona fide cases of IgG4-RD are associated with normal IgG4 serum levels, while elevated levels are sometimes observed in simulators such as RDD. The threshold of IgG4-positive cells per hpf varies by organ and by set of criteria. Furthermore, many diseases are associated with large numbers of IgG4-positive plasma cells. For example, a significant percentage of GF cases will meet criteria for IgG4-RD when relying on this criterion. For these reasons, the histopathologic features (lymphoplasmacytic infiltrates, storiform fibrosis, obliterative phlebitis, and eosinophils) along with clinicopathologic correlation are more important than the percentage or absolute number of IgG4-positive plasma cells. This understanding can reduce overdiagnosis of IgG4-RD and misdiagnosis of more common skin diseases.
The 2020 Revised comprehensive diagnostic (RCD) criteria for IgG4-RD (3)
Clinical and radiological features
One or more organs show diffuse or localized swelling or a mass or nodule characteristic of IgG4-RD. In single organ involvement, lymph node swelling is omitted.Serological diagnosis
Serum IgG4 levels greater than 135 mg/dl.Pathological diagnosis
Positivity for two of the following three criteria:Dense lymphocyte and plasma cell infiltration with fibrosis.
Ratio of IgG4-positive plasma cells /IgG-positive cells greater than 40% and the number of IgG4-positive plasma cells greater than 10 per high powered field
Typical tissue fibrosis, particularly storiform fibrosis, or obliterative phlebitis
Diagnosis:
Definite: 1) + 2) + 3)
Probable: 1) + 3)
Possible: 1) + 2)
The reader is advised to read reference 3 by Umehara et al. detailing explanatory notes on proper usage of these criteria. This may also be compared with the 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease (Wallace ZS et al. American College of Rheumatology/European League Against Rheumatism IgG4-Related Disease Classification Criteria Working Group. The 2019 American College of Rheumatology/European League Against Rheumatism Classification Criteria for IgG4-Related Disease. Arthritis Rheumatol. 2020 Jan;72(1):7-19. doi: 10.1002/art.41120. Epub 2019 Dec 2. PMID: 31793250.)
References
Nambiar S, Oliver TI. IgG4-Related Disease. 2023 Aug 8. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan–. PMID: 29763000.
Katz G, Stone JH. Clinical Perspectives on IgG4-Related Disease and Its Classification. Annu Rev Med. 2022 Jan 27;73:545-562. doi: 10.1146/annurev-med-050219-034449. Epub 2021 Oct 20. PMID: 34669430.
Umehara H, Okazaki K, Kawa S, Takahashi H, Goto H, Matsui S, Ishizaka N, Akamizu T, Sato Y, Kawano M; Research Program for Intractable Disease by the Ministry of Health, Labor and Welfare (MHLW) Japan. The 2020 revised comprehensive diagnostic (RCD) criteria for IgG4-RD. Mod Rheumatol. 2021 May;31(3):529-533. doi: 10.1080/14397595.2020.1859710. Epub 2021 Jan 28. PMID: 33274670.
Tokura Y, Yagi H, Yanaguchi H, Majima Y, Kasuya A, Ito T, Maekawa M, Hashizume H. IgG4-related skin disease. Br J Dermatol. 2014 Nov;171(5):959-67. doi: 10.1111/bjd.13296. Epub 2014 Oct 20. PMID: 25065694.
Mishlab S, Bergman R, Hersh EA. Cutaneous IgG4-related disease. Int J Dermatol 2022; 62: 556-561.
Akatsuka T, Matsuoka A, Norimatsu Y, Morimura S, Hamada T, Matsuoka R, Hayashi Y, Soga H, Usui T, Sugaya M. A case of IgG4-related disease presenting as skin tumors in the bilateral cheeks. J Dermatol. 2024 Oct;51(10):e358-e359. doi: 10.1111/1346-8138.17271. Epub 2024 May 17. PMID: 38760966.
Gitin A, Patel SP, Weatherall A, Vincek V, Motaparthi K. Xanthomatous cutaneous Rosai-Dorfman disease with overlapping features of IgG4-related disease. JAAD Case Rep. 2022 Sep 15;29:134-138. doi: 10.1016/j.jdcr.2022.09.004. PMID: 36262360; PMCID: PMC9574542.
Skopec Z, Alsawas M, Maxwell T, Pelletier D, Brown-Joel Z, Bellizzi A, Liu V. Assessment of specificity of dermatopathologic criteria for IgG4-related skin disease. J Cutan Pathol. 2024 Feb;51(2):163-169. doi: 10.1111/cup.14548. Epub 2023 Oct 18. PMID: 37853944.
Beck TC, Plante J, Robinson I, Khatskevich K, Forcucci JA, Valdebran M. Immunoglobulin G4-Related Disease-Associated Dermatitis with Pruritus: A Positive Response to Dupilumab. Life (Basel). 2023 Mar 20;13(3):833. doi: 10.3390/life13030833. PMID: 36983988; PMCID: PMC10056512.
Spiera R. Beyond Glucocorticoids for IgG4-Related Disease. N Engl J Med. 2025 Mar 27;392(12):1232-1233. doi: 10.1056/NEJMe2413286. PMID: 40138558.
Stone JH, Khosroshahi A, Zhang W, Della Torre E, Okazaki K, Tanaka Y, Löhr JM, Schleinitz N, Dong L, Umehara H, Lanzillotta M, Wallace ZS, Ebbo M, Webster GJ, Martinez Valle F, Nayar MK, Perugino CA, Rebours V, Dong X, Wu Y, Li Q, Rampal N, Cimbora D, Culver EL; MITIGATE Trial Investigators. Inebilizumab for Treatment of IgG4-Related Disease. N Engl J Med. 2025 Mar 27;392(12):1168-1177. doi: 10.1056/NEJMoa2409712. Epub 2024 Nov 14. PMID: 39541094.
Stone JH. IgG4-related disease: lessons from the first 20 years. Rheumatology (Oxford). 2025 Mar 1;64(Supplement_1):i24-i27. doi: 10.1093/rheumatology/keaf008. PMID: 40071397.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
posted by dermatica at
December 16, 2025
![]()
![]()

0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home