Leishmania y CD1a
LEISHMANIA EPISODE 1A: ATTACK OF THE CLONES

By Kiran Motaparthi, MD
February 10, 2021
Vol. 3, No. 6

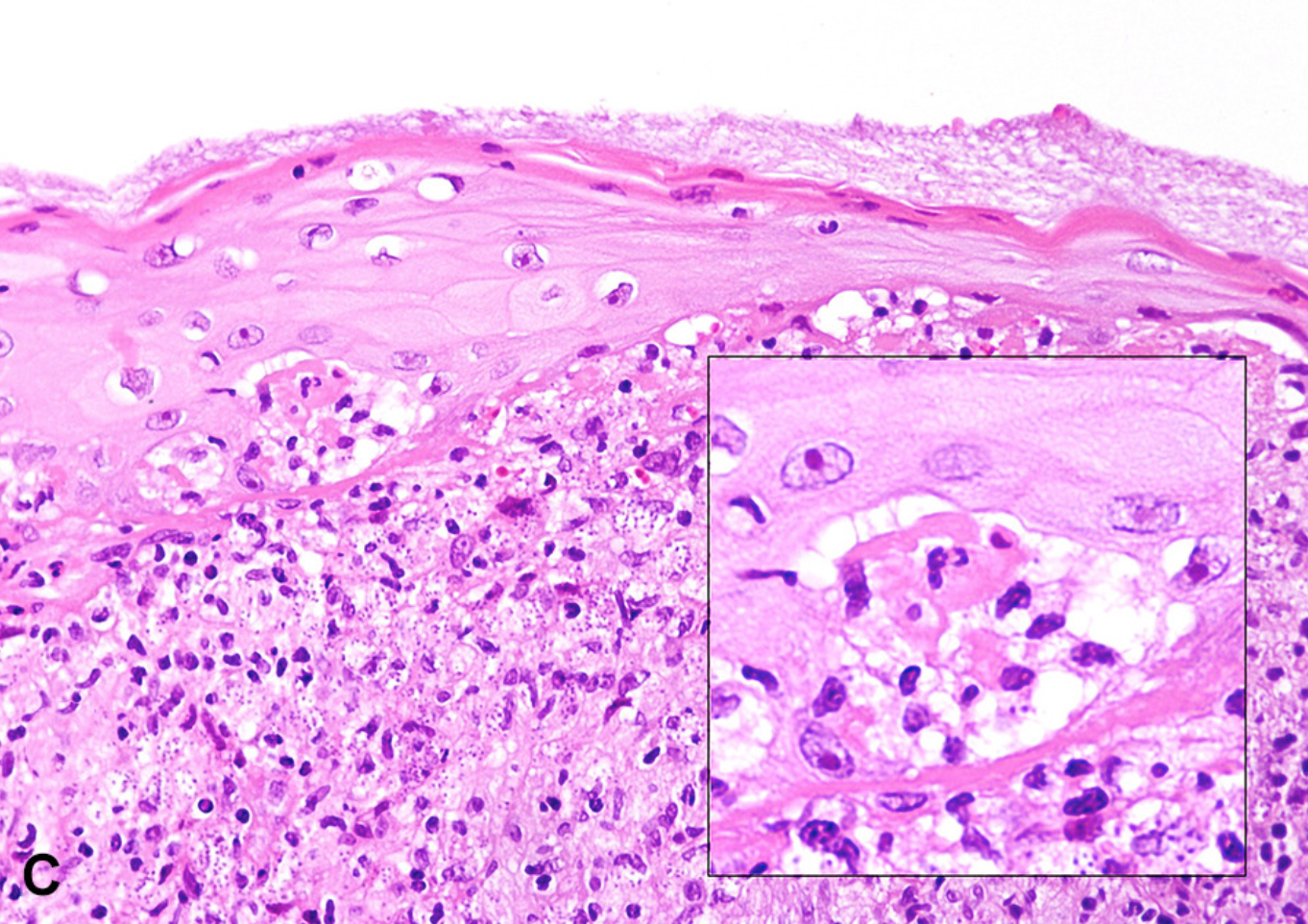
Recently, CD1a immunostain has been used to identify amastigotes (Figure 1), demonstrating a peripheral "membrane-like" pattern with accentuation in one of the poles, leaving the unstained nucleus in the center (Figure 2). (4, 5) As antigen-presenting cells, Langerhans cells (CD1a-positive dendritic cells) phagocytize amastigotes before triggering T-cell mediated immunity. Most likely, antigen transfer of CD1a occurs during exocytosis. Alternatively, there may exist cross-reactivity between surface antigens of Leishmania and the CD1a epitope. However, this is less likely given that promastigotes cultured outside of hosts are CD1a-negative. (3, 5)

However, there are several caveats with the practical or routine use of this antibody stain:
There is variability in sensitivity based on the clone of anti-CD1a antibody used: MTB1 (Novocastra/Leica Biosystems) is variably positive depending on the species of Leishmania, but the clone 010 (Dako) is consistently negative. (5)
The species and hence geographic region influence detection by this method: CD1a (MTB1) is highly sensitive for the detection of L. infantum, (5) L. tropica, and L. major. (4) CD1a (MTB1) can also enable diagnostic confirmation in cases of Old World CL without identifiable amastigotes on H&E-stained sections. (6) However, CD1a (MTB1) is variably sensitive for New World species such as L. panamensis (3) and insensitive for L. braziliensis and L. peruviana. (7)
If amastigotes encounter Langerhans cells in the epidermis or papillary dermis, antigen transfer can occur. However, amastigotes that are injected into the deep dermis or new populations of amastigotes are less likely to be processed by CD1a-positive dendritic cells and will therefore be CD1a-negative. (3,5)
As with any stain, technical and interpretive difficulties may arise. Rare amastigotes present in H&E-stained sections may be lost in sections prepared for CD1a staining. (7) Dendritic cell cytoplasmic prolongations may mimic CD1a-positive organisms, appearing as oval fragments the size of amastigotes. (8)
Superior methods for detection of Leishmania are readily available in the United States. Culture and polymerase chain reaction (PCR) are up to 80% and 97% sensitive, respectively, and permit definitive diagnosis in challenging cases without identifiable organisms. Of importance for treatment selection, PCR permits speciation. (2) If a dermatologist suspects CL, at least 2 punch biopsies should be obtained: 1 for histopathology and 1 for PCR and culture. While the biopsy for histopathology should be placed in formalin, the biopsy for PCR/culture should be placed in a non-fixative preservative such as Roswell Park Institute Medium or buffered saline. The CDC provides media, histopathology, PCR, and culture free of charge. (9) See resources and instructions from the CDC (PDF).
Point to Remember: When a trained eye and routine H&E-stained sections are insufficient, PCR increases the diagnostic yield and may influence therapy. In settings where access to PCR and culture are limited, the use of a specific CD1a clone (MTB1) is sensitive for the detection of Old World species and provides variable support for the diagnosis of New World disease.
Our editor's viewpoint
Warren R. Heymann, MD
As I am writing this commentary travel bans are in effect related to the coronavirus situation. I hope that by the time this is published, that epidemic is under control, and that people can again travel worldwide without restriction. Under normal circumstances any dermatologist can see tropical disorders, leishmaniasis being among the most frequent. I have diagnosed cases — both New World and Old World — in my career. I cannot say enough about how obliging the CDC is in assisting with the diagnosis and treatment of patients with cutaneous leishmaniasis. By all means, request a CD1a stain if the H&E is equivocal and your suspicion is high for cutaneous leishmaniasis. Your next step, post haste, is to contact the CDC.
Taxy JB, Goldin HM, Dickie S, Cibull T. Cutaneous Leishmaniasis: Contribution of Routine Histopathology in Unexpected Encounters. Am J Surg Pathol. 2019;43(2):195–200.
Handler M, Patel P, Kapila R, Al-Qubati Y, et al. Cutaneous and mucocutaneous leishmaniasis. J Am Acad Derm. 2015;73(6):911–26.
Sundharkrishnan L, North JP. Histopathologic features of cutaneous leishmaniasis and use of CD1a staining for amastigotes in Old World and New World leishmaniasis. J Cutan Pathol. 2017;44(12):1005-1011.
Jabbour MN, Issa G, Charafeddine K, Simaan Y, et al. The immune microenvironment in cutaneous leishmaniasis. J Eur Acad Dermatol Venereol. 2015;29(6):1170–1179.
Fernandez-Flores A, Rodriguez-Peralto JL. Morphological and immunohistochemical clues for the diagnosis of cutaneous leishmaniasis and the interpretation of CD1a status. J Am Acad Dermatol. 2016;74(3):536-43.
Dias-Polak D, Geffen Y, Ben-Izhak O, Bergman R. The Role of Histopathology and Immunohistochemistry in the Diagnosis of Cutaneous Leishmaniasis Without "Discernible" Leishman-Donovan Bodies. Am J Dermatopathol. 2017;39(12):890–895.
Ferrufino-Schmidt MC, Bravo F, Valencia BM, Llanos-Cuentas A, et al. Is CD1a useful for leishmaniasis diagnosis in the New World?. J Cutan Pathol. 2019;46(1):90–92.
Fernandez-Flores A. A new scenario in the immunohistochemical diagnosis of cutaneous leishmaniasis. J Cutan Pathol. 2017;44(12):1051–1052.
Centers for disease control and prevention: practical guide for specimen collection and reference diagnosis of leishmaniasis (Online). 2016. Available at: https://www.cdc.gov/parasites/leishmaniasis/resources/pdf/cdc_diagnosis_guide_leishmaniasis_2016.pdf Accessed 24 February 2020.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
DW Insights and Inquiries archive
Explore hundreds of Dermatology World Insights and Inquiries articles by clinical area, specific condition, or medical journal source
Skin Care Physicians of Costa Rica
Clinica Victoria en San Pedro: 4000-1054
Momentum Escazu: 2101-9574
Please excuse the shortness of this message, as it has been sent from
a mobile device.
posted by dermatica at
February 10, 2021
![]()
![]()

0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home