POSITIVELY PERPLEXING: DETERMINING THE MEANING OF CD30 POSITIVITY
By Warren R. Heymann, MD, FAAD
Sept. 29, 2021
Vol. 3, No. 39
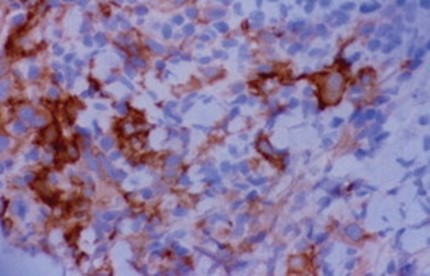
Primary cutaneous CD30+ T-cell lymphoproliferative disorders (CD30+ LPD) are the second most common cutaneous lymphomas after mycosis fungoides (MF) and Sézary syndrome (SS), representing approximately 30% of all cutaneous lymphomas. According to the World Health Organization (WHO), CD30+ LPD include primary cutaneous anaplastic large cell lymphoma (pcALCL), lymphomatoid papulosis (LyP), and borderline lesions. LyP and pcALCL represent two poles of a spectrum of diseases with different clinical presentations, clinical courses, and prognosis. Regardless, both entities display overlapping histopathologic and immunophenotypic features, which can render the diagnosis of borderline lesions difficult. CD30 positivity may also be observed in large cell transformation in MF, Hodgkin lymphoma, and other reactive disorders. (1)
CD30 is a transmembrane glycoprotein receptor of the tumor necrosis factor receptor super family 8 (TNFRSF8), mediating its effects through a number of signaling pathways that produce a survival advantage to the cells on which the protein is overexpressed. Stimulation of CD30 leads signal mediation through tumor necrosis factor receptor-associated proteins (TRAF), thereby stimulating the nuclear factor-kappa B (NFkB) pathway and the mitogen-activated protein kinase (MAPK) pathways. In reactive conditions, CD30 receptor and ligand (CD30L, CD153) expression is normally seen on activated T-immunoblasts and B-immunoblasts. (2)
It cannot be overemphasized that the presence of CD30+ cells does not equate with neoplasia, in the same way that clonality does not confer the diagnosis of cancer. (1) CD30+ infiltrates may be observed in, but are not limited to, infections (Milker's nodule, HSV, VZV, molluscum, scabies, leishmaniasis, syphilis), inflammatory conditions (lymphomatoid drug reactions, pernio), ruptured cysts, and re-excision of neoplasms. Xu et al state that "there is no standardized or validated form of performing the interpretation of CD30 expression." (2)
The pitfalls in diagnosing cutaneous lymphoma are so numerous, one wonders if any dermatopathologist can get a good night's sleep. These pitfalls have been reviewed in the valuable article by Batrani and Bhawan and include diagnostic traps in morphology (such as the presence or lack of epidermotropism), angioinvasion/angiocentricity, subcutaneous lymphoid rimming of adipocytes, immunohistochemistry (including CD30; absence/loss of pan B-cell and pan T-cell antigens), reactive cell population of other lineage, aberrant antigen expression, gene rearrangement studies, lineage infidelity, dual clones, and composite lymphomas. (3)
Pernio has been in the news (see David Wetter's commentary in DWI&I). Ample attention has been paid to "COVID toes" and its potential relationship to "routine" pernio and the SARS-CoV-2 virus. Hernandez and Bruckner state: "It is still unclear whether a viral cytopathic process vs a viral reaction pattern or other mechanism is responsible for "COVD toes." (4) Histologically, both idiopathic and secondary pernio (associated with lupus, Raynaud phenomenon, acrocyanosis, and livedoid vasculopathy) both display variable interface dermatitis, papillary dermal edema, and a superficial and deep perivascular and periadnexal infiltrate, composed mostly of T-cells. (5)
Dany et al reported the case of a 31-year-old woman with a history of rheumatoid arthritis and pernio. Histologically, it was noted that 20% of her cells were atypical, staining positive for CD30. The authors reviewed the literature, finding 3 similar cases, referring to the senior authors' prior observation of CD30 positivity in 2 cases of pernio (a 16-year-old healthy adolescent woman and a 67-year-old woman with Raynaud phenomenon). Both of these latter patients improved with warm weather. Massey et al assert: "Our cases highlight the importance of clinicopathologic correlation in the assessment of CD30 positive lymphocytes in benign nonneoplastic conditions. The clinical presentation of symptomatic papular or nodular lesions made worse by cold and remitting in warmer temperatures was consistent with perniosis. Clinicians and pathologists should be cautioned not to overinterpret CD30 positive cells in otherwise reactive processes." (6)
Although I agree completely with Massey et al, the overarching lesson is exactly the same since dermatologists first used microscopy — when it comes to clinicopathologic correlation, living morphology takes precedence over all else. Unexpected outcomes may arise. Look at the patient. Follow the patient. Re-biopsy if necessary. At the risk of sounding like an Abbott and Costello routine, while it is important to be cognizant of pitfalls, a pitfall of pitfalls is in recognizing that on rare occasions, what was interpreted as a pitfall may not be a pitfall after all. Think about it.
Point to Remember: Clinicopathologic correlation is the key to interpreting histopathology in lymphoproliferative disorders. The presence of CD30 positivity does not confer the diagnosis of a CD30+ lymphoproliferative disorder. Upon receiving a biopsy report noting the presence of CD30+ cells, careful thought and clinical follow-up are essential in determining if lesions are reactive or neoplastic.
Our expert's viewpoint
Rosalie Elenitsas, MD, FAAD
Herman Beerman Professor
Director, Dermatopathology
University of Pennsylvania Perelman School of Medicine
Every day we are challenged in the practice of medicine trying to decide which findings are important to the patient's diagnosis and which may be insignificant. This also happens at the microscope when dermatopathologists have to decide which cells are pertinent to the diagnosis and which are irrelevant. A wise trainee once asked me, "Is that a skipocyte?" They were referring to a cell that we skip or ignore. Identifying, or more appropriately NOT identifying, the "skipocytes" is the art of pathology. It can be learned by viewing many slides and keeping abreast of the medical literature. Tim McCalmont's editorial "Red alert or red herring" addressed the presence or absence of eosinophils in dermatopathology. As he notes, sometimes eosinophils can be the clue to the diagnosis and other times they are just along for the ride. The literature and our experiences help us determine when that cell deserves attention. Similarly, the presence of enlarged CD30-positive lymphocytes in a skin biopsy pose an analogous problem. In addition to CD30 lymphoproliferative diseases, there is growing literature on reactive infiltrates with these large activated T cells. My personal experience is that hypersensitivity reactions are the most common, such as reactions to insect bites and medications, but the list includes many unrelated disease categories. It is important to be aware of this concept of reactive CD30 positive lymphocytes. If there is clinical-pathological disparity, dermatologists should not hesitate to take a second biopsy or discuss the case with their pathologist.
Di Raimondo C, Parekh V, Song JY, Rosen ST, Querfeld C, Zain J, Martinez XU, Abdulla FR. Primary Cutaneous CD30+ Lymphoproliferative Disorders: a Comprehensive Review. Curr Hematol Malig Rep. 2020 Aug;15(4):333-342. doi: 10.1007/s11899-020-00583-4. PMID: 32435988.
Xu ML, Gabali A, Hsi ED, Fedoriw Y, Vij K, Salama ME, Ramchandren R, O'Malley D, Wick MR, Battistella M, Gru AA. Practical Approaches on CD30 Detection and Reporting in Lymphoma Diagnosis. Am J Surg Pathol. 2020 Feb;44(2):e1-e14. doi: 10.1097/PAS.0000000000001368. PMID: 31567279.
Batrani M, Bhawan J. Pitfalls in the diagnosis of cutaneous lymphoma. Am J Dermatopathol. 2014 Jan;36(1):90-100. doi: 10.1097/DAD.0b013e31827654cd. PMID: 24366200
Hernandez C, Bruckner AL. Focus on "COVID toes". JAMA Dermatol 2020; 156: 1003.
Dany M, Fischer AS, Mollanazar NK, Rubin AI, Elenitsas R. CD30-positive atypical lymphocytes in perniosis: a potential diagnostic pitfall in a benign inflammatory dermatosis. J Cutan Pathol. 2020 Sep;47(9):781-784. doi: 10.1111/cup.13697. PMID: 32815227.
Massey PR, Wanat KA, Stewart CL, Kim EJ, Castelo-Soccio L, Elenitsas R, Rubin AI. CD30 positive atypical lymphocytes in perniosis: a potential histopathologic pitfall in a benign condition. Am J Dermatopathol. 2014 Sep;36(9):730-3. doi: 10.1097/DAD.0000000000000109. PMID: 25072680.
McCalmont TH. Red alert or red herring? J Cutan Pathol 2014:41:337-339.
Skin Care Physicians of Costa Rica
Clinica Victoria en San Pedro: 4000-1054
Momentum Escazu: 2101-9574
Please excuse the shortness of this message, as it has been sent from
a mobile device.
posted by dermatica at
October 09, 2021
![]()
![]()


0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home