GRANULAR DETAIL ON GRANULAR PARAKERATOSIS

By Warren R. Heymann, MD, FAAD
October 6, 2021
Vol. 3, No. 40
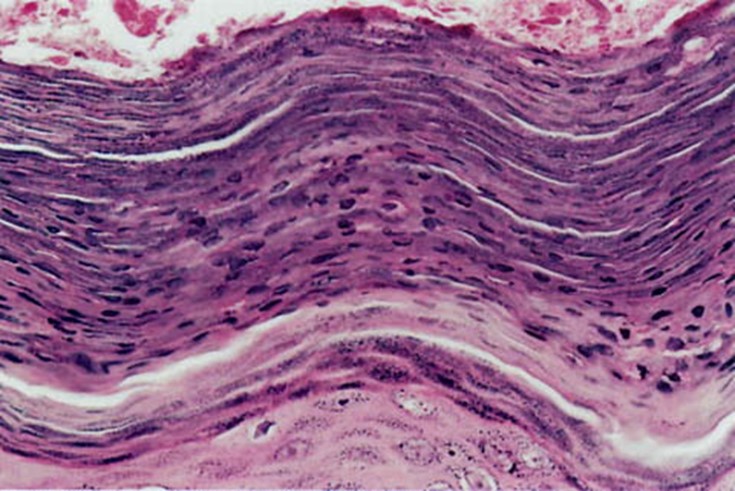
The term axillary granular parakeratosis is proposed for a unique axillary eruption with distinct histopathologic features. Four middle-aged to elderly patients (three women, one man) had unilateral or bilateral, usually pruritic, hyperpigmented to bright red patches in the axillae. Biopsy specimens revealed severe compact parakeratosis with the stratum corneum measuring 80 to 250 microns in maximal thickness, maintenance of the stratum granulosum, remarkable retention of keratohyaline granules throughout the stratum corneum, and vascular proliferation and ectasia. A contact reaction to an antiperspirant/deodorant is suspected as the cause. We speculate that the offending agent alters the maturation sequence of the stratum granulosum and stratum corneum, possibly by interfering with the degradation of filaggrin precursor to filaggrin units.
The disorder is now referred to as granular parakeratosis (GP) because of its presence at other (mostly flexural) sites. GP occurs in all ages but is most commonly seen in adults. Patients with GP characteristically present with asymptomatic to pruritic papules or plaques in intertriginous areas. Lesions are typically reddish to brown and present as scaly-to-keratotic papules that may coalesce into plaques in intertriginous areas such as the axillae, submammary folds, abdominal folds, or inguinal folds. In children GP presents as linear plaques in the bilateral inguinal folds or as geometric plaques in areas of increased pressure during diaper-wearing. Granular parakeratosis has not been associated with any systemic diseases. (2)
The clinical differential diagnosis includes intertrigo, Hailey-Hailey disease, Darier disease, pemphigus vegetans, confluent and reticulated papillomatosis, acanthosis nigricans, seborrheic keratoses, and irritant or allergic contact dermatitis. The diagnosis of GP is confirmed histologically marked compact parakeratotic horn with retention of keratohyalin granules. (3)

In a letter to the editor regarding the article by Shen et al, Kumarasinghe et al report that in their experience similar cases were observed in patients who have not used any benzalkonium chloride-containing laundry detergents. They also propose the term hyperkeratotic flexural erythema (HKFE) to encompass all cases of this clinical entity based on the observation that GP may or may not be present on all biopsies. The authors suggest that disordered keratinization of HKFE may be due to a change in the flexural microbiome due to irritants or other causes. (5)
Therapeutically, most cases will respond to removal of the trigger (usually an antiperspirant) with concurrent use of topical steroids. Therapeutic success has also been reported with vitamin D analogues, topical or oral retinoids, ammonium lactate, calcineurin inhibitors, topical or oral antifungals, cryotherapy, and botulinum toxin injections. (3,6)
My interest in GP was rekindled after reading the article by Fujii et al detailing their mouse model where topical aluminum chloride caused apoptosis, maturation arrest, and GP. (7). The following is the abstract of the article.
Aluminum chloride (AlCl3) is the main active ingredient in commonly used antiperspirant. Antiperspirant use may cause a rare keratinization disease, granular parakeratosis (GP), then AlCl3 may be associated with the etiology of GP. The objective of this study is to elucidate the skin effect of topical aluminum application using a mouse model. We sprayed 20% aluminum chloride every day on the depilated mice skin and analyzed the skin clinically, histopathologically, and immunohistologically. We have succeeded in the histological replication of GP on mouse skin. The basophilic granules in the stratum corneum contained filaggrin, and processing of profilaggrin to filaggrin was disrupted in aluminum-treated mouse skin (Al-mouse). In Al-mouse, cytochrome c and cleaved-caspase 3 were upregulated mainly in the granular layer, and caspase 3 p20 subunit was upregulated. TUNEL-positive cells increased significantly in the Al-mouse from the granular to the horny layer. Caspase 3 inhibitor inhibited granular parakeratotic change of Al-mouse. Our results indicated that aluminum-induced apoptosis leads to keratinization arrest and acceleration of nuclear degradation before completion of profilaggrin processing. This could lead to retention of the basophilic granules composed of underprocessed profilaggrin in the horny layer of Al-mouse skin, the hallmark of GP.
It is fascinating to ponder how topical caspase inhibitors may affect other disorders of keratinization. Most importantly, I encourage you to reread the abstract by Northcutt et al — I was awestruck by their prescience and brilliance. It serves as a reminder that every dermatologist has the opportunity to carefully examine patients making novel observations which may open new vistas of diagnosis and therapy.
Point to Remember: Granular parakeratosis may affect all age groups and usually responds to removal of the potential irritant with straightforward topical therapy. A mouse model of GP raises intriguing possibilities about pathogenesis and potential new therapies for disorders of keratinization.
Our expert's viewpoint
Christen Mowad, MD, FAAD
Chair of Dermatology, Geisinger Medical Center
This was a very timely commentary as I had just seen a 54-year-old Caucasian women with a several month history of an itchy rash in both axilla. She denied a new deodorant but had just purchased a new container of it. The eruption was a characteristic brownish keratotic set of papules coalescing into plaques with some maceration involving both axillae. This eruption known as granular parakeratosis has these characteristic clinical features and occurs most commonly in women and typically in adults. It is usually localized to intertriginous sites. There is an infantile presentation associated with diapers involving the inguinal folds. The pathology is characteristic and demonstrates retention of basophilic keratohyaline granules and parakeratosis. The pathophysiology of this eruption has been linked to an allergic contact dermatitis as well as occlusion, maceration, and friction. It appears that an abnormality in keratinization occurs either from an underlying defect in filaggrin or a change in the microbiome or a change in the keratinization process due to irritants. The recent article demonstrating aluminum chloride as a cause of apoptosis and keratinization arrest and granular parakeratosis is intriguing. The awareness of this condition when considering the differential diagnosis of the clinical picture is important. Treatment typically involves removal of the antiperspirant and topical agents. The effect of aluminum chloride and other topical agents on keratinization is fascinating and may be a key to treating keratinization disorders. Though not yet crystal clear the granules of this disorder are being put together and may go far beyond the understanding of just this entity.
All content found on Dermatology World Insights and Inquiries, including: text, images, video, audio, or other formats, were created for informational purposes only. The content represents the opinions of the authors and should not be interpreted as the official AAD position on any topic addressed. It is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
Skin Care Physicians of Costa Rica
Clinica Victoria en San Pedro: 4000-1054
Momentum Escazu: 2101-9574
Please excuse the shortness of this message, as it has been sent from
a mobile device.

0 Comments:
Post a Comment
Subscribe to Post Comments [Atom]
<< Home